Type 1 diabetes Autoimmune
Being Aware of Type 1 Diabetes: Symptoms, Causes, and Management
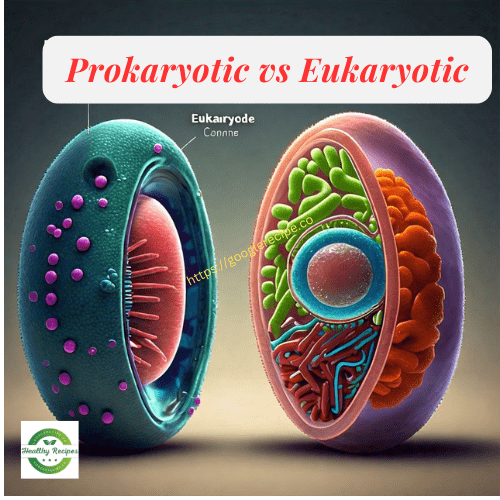
We’ll talk about type 1 autoimmune diabetes. This type of diabetes destroys the pancreatic beta cells, which produce insulin. Without enough insulin, the body’s blood sugar levels rise, and glucose doesn’t get properly used by tissues. Before diving into the details of type 1 diabetes and its complex immune responses, let’s start with the basics.
You’ve probably heard the term “sugar” from your parents or grandparents. The medical term for high blood sugar is diabetes. Diabetes means elevated blood sugar levels, which can have serious consequences.
But why is high blood sugar bad? Our bodies use carbohydrates, proteins, and fats for fuel, preferring carbohydrates. Carbohydrates and glucose aren’t bad themselves. The problem is when the body can’t use glucose properly.
Blood glucose levels
In diabetes, there’s glucose, but the body can’t use it. Normally, after eating, blood glucose levels rise, and glucose moves to muscles, liver, or fat tissues for use. But for someone with diabetes, this process doesn’t happen correctly. Even if glucose is present, the body can’t utilize it, leading to complications. Excess glucose in the blood can have severe consequences.
There are many reasons for diabetes, and over 30 million people in the U.S. are affected by it annually. Diabetes-related medications cost about $100 billion every year. The situation is severe worldwide, with increasing incidence in South Asia and the Western Pacific.
Eat a meal high in glucose
Let’s say you eat a meal high in glucose. Normally, your blood glucose level increases, then decreases as your body uses the glucose. In a diabetic person, blood glucose levels rise and stay high because the body can’t move glucose effectively. Pancreatic beta cells secrete insulin, a hormone crucial for glucose movement. If these cells are destroyed, insulin levels drop.
There are two main types of diabetes. In type 1 diabetes, the body can’t produce insulin due to the destruction of beta cells. In type 2 diabetes, the body becomes resistant to insulin, meaning it can’t respond to insulin. Our focus here is type 1 diabetes. Genetic factors and immune responses cause type 1 diabetes. One major factor is the human leukocyte antigen, which produces molecules associated with diabetes.
Treats pancreatic beta cells
In type 1 diabetes, the body mistakenly treats pancreatic beta cells as foreign and produces autoantibodies against them. These autoantibodies are recognized by immune cells like macrophages and dendritic cells, leading to inflammation. Cytotoxic T cells then destroy the beta cells. Once these cells are destroyed, insulin production drops, leading to high blood glucose levels and severe consequences.
There are solutions to type 1 diabetes, with one primary solution being external insulin. After meals, the body needs insulin to move glucose, and since it can’t produce enough, external insulin helps.
The stages of type 1 diabetes are: genetic risk, immune activation, immune response, and detection phases. People with certain genetic makeups are more susceptible to type 1 diabetes.
Conclusion
Type 1 autoimmune diabetes is a serious condition resulting from the destruction of pancreatic beta cells, leading to a lack of insulin and high blood glucose levels. Understanding the basic mechanics of this disease helps us appreciate the importance of insulin in regulating blood sugar and the severe consequences when the body cannot utilize glucose properly.
With millions affected globally and the incidence rising, it’s crucial to be aware of the genetic and immune factors contributing to type 1 diabetes. While external insulin remains a primary treatment, ongoing research and advancements are essential for better management and potential cures.
By understanding and addressing the complexities of type 1 diabetes, we can improve the quality of life for those affected and work towards reducing its global impact.
FAQs
Q: What causes type 1 diabetes? A: Type 1 diabetes is caused by the immune system attacking and destroying the insulin-producing beta cells in the pancreas. This autoimmune response can be triggered by genetic and environmental factors.
Q: How is type 1 diabetes different from type 2 diabetes? A: In type 1 diabetes, the body cannot produce insulin due to the destruction of beta cells. In type 2 diabetes, the body becomes resistant to insulin, meaning it can’t use insulin effectively, even though it is still produced.
Q: Can type 1 diabetes be prevented? A: There’s no known treatment to stop type 1 diabetes at this time.. Researchers are studying the disease to understand its causes and develop potential preventive measures.
Q: What are the symptoms of type 1 diabetes? A: Symptoms include frequent urination, extreme thirst, unexplained weight loss, fatigue, blurred vision, and increased hunger.
Q: How is type 1 diabetes managed? A: Type 1 diabetes is managed through regular blood sugar monitoring, insulin therapy, a balanced diet, and regular physical activity. Working closely with a healthcare team can help manage the condition effectively.